Introduction — Why inflammation is now front-page health news
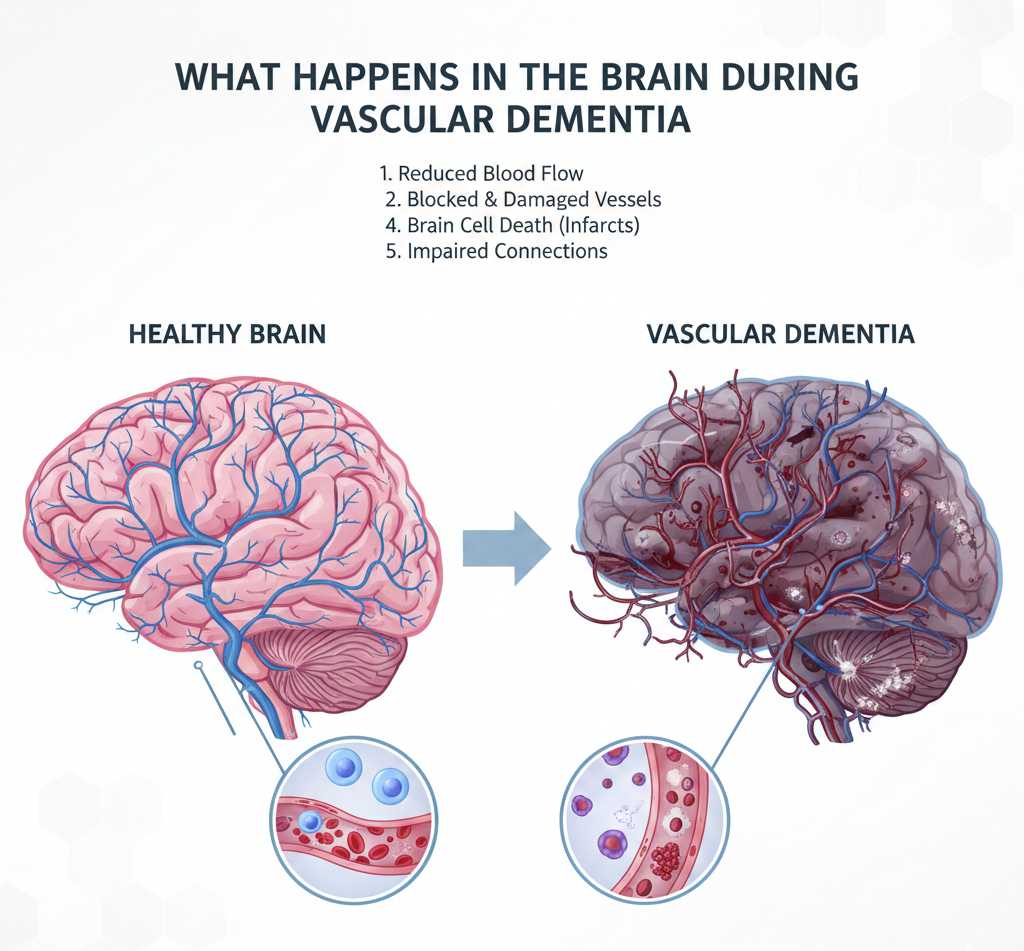
“Inflammation” has moved from a technical medical term to a dominant frame in health conversations. Once mainly discussed within rheumatology and acute infection care, inflammation is now widely presented as a common biological thread linking cardiovascular disease, metabolic disorders such as type 2 diabetes, some cancers, and neurodegenerative conditions. Multiple new reports and analyses — including market forecasts, clinical trial outcomes and nutrition research — point to rising interest from consumers, clinicians and industry in strategies to measure, prevent and treat chronic inflammation. This article unpacks what that interest means and why it is accelerating now.
What the new reports show
Several market research firms and industry analysts have recently published outlooks emphasizing growth across the anti-inflammatory category. These reports aggregate data from prescription sales, over-the-counter analgesics, nutraceuticals and emerging biologic pipelines to show rising revenues, expanding clinical trial activity and increasing investor attention. The big-picture signal is consistent: a multi-pronged uptick in demand for interventions that explicitly target inflammatory pathways or that claim to reduce inflammatory burden.
Key drivers cited across reports include an aging population, higher diagnosis rates of chronic inflammatory conditions, broader consumer interest in preventive health, and accelerating R&D in targeted immunomodulatory therapies.
Market segments: Where the growth is happening
Pharmaceuticals and biologics
The pharmaceutical industry is experiencing concentrated investment in targeted inflammation modulators. Biologic agents — monoclonal antibodies and other large-molecule therapies — have already transformed outcomes for rheumatoid arthritis, inflammatory bowel disease and psoriasis. Newer entrants aim at more precise cytokine targets, intracellular signaling proteins, and cell-based therapies. These high-cost drugs drive attention because of their clinical effectiveness and lucrative market value, even as access and affordability remain challenges.
Over-the-counter and prescription NSAIDs
NSAIDs (non-steroidal anti-inflammatory drugs) remain a major, well-established category. OTC formulations continue to be widely used for short-term pain and inflammation, while prescription-level NSAIDs and COX-2 selective agents fill ongoing clinical needs. Market analyses show steady sales in mature markets and growth in regions with rising healthcare access.
Supplements and functional foods
Parallel to pharmaceutical trends, consumer markets for anti-inflammatory supplements — omega-3s, curcumin extracts, polyphenol-rich products and joint-support formulations — have expanded rapidly. Functional food products marketed with anti-inflammatory claims (fortified beverages, plant-based meal kits) are increasingly common in e-commerce and retail channels.
Clinical research: Why clinicians are paying attention
Clinicians’ interest is shaped by accumulating evidence that chronic, low-grade inflammation contributes to long-term disease risk. Large observational studies and controlled trials have linked elevated inflammatory biomarkers (for example, hs-CRP, IL-6) to cardiovascular events, metabolic dysfunction and poorer outcomes in diverse patient populations. Importantly, interventional trials that reduce specific inflammatory mediators have, in certain cases, delivered measurable clinical benefit — a fact that underscores the therapeutic potential of anti-inflammatory approaches beyond symptom control.
That said, the clinical community also emphasizes nuance: inflammation is a multifaceted biological process. Therapeutic approaches must be tailored to disease mechanism, severity and patient risk profile. Biomarker-guided prescribing and targeted immunomodulation are emerging as preferred models rather than blanket anti-inflammatory prescriptions for broad prevention.
Nutrition and lifestyle: The population-level lever
Growing research on diet, physical activity and other lifestyle factors has validated the idea that everyday choices influence baseline inflammatory burden. Dietary patterns rich in fruits, vegetables, whole grains, legumes, nuts, and fatty fish — and low in processed meats, refined sugars and ultra-processed foods — are associated with lower levels of systemic inflammatory markers. Several research groups have worked to quantify an “anti-inflammatory diet index” and to test whether structured dietary interventions reduce inflammation-related outcomes.
For public health, lifestyle interventions represent a scalable, low-cost opportunity. However, translating promising study results into large-scale, equitable programs requires policy action to improve food environments, subsidize healthy foods, and integrate nutrition counseling into routine care.
Supplements: Promise, hype and regulation
The supplement space is particularly contested. Some ingredients (notably long-chain omega-3 fatty acids) have a substantive trial evidence base for specific conditions, while others are supported mainly by smaller or inconsistent human studies. Consumers gravitate to supplements because they offer an approachable, lower-perceived-risk route to “reduce inflammation,” but variability in product quality, dosing, and bioavailability is a major concern.
Regulators and professional societies commonly recommend caution: use evidence-backed formulations, prefer third-party quality certification, and discuss supplement use with healthcare providers — especially when combining supplements with prescription anti-inflammatory medicines to avoid interactions and compounded risks.
Safety and long-term trade-offs
Increased use of anti-inflammatory strategies raises important safety questions. Chronic use of certain NSAIDs is associated with renal, gastrointestinal and cardiovascular risks. Immune-targeting biologics can raise infection risk and require monitoring for adverse effects. Even seemingly benign supplements can interact with medications (for example, omega-3s and anticoagulants) or contain variable amounts of active compounds.
Because of these trade-offs, experts stress evidence-based, individualized decision-making: targeted use of pharmacologic therapies where indicated, broader lifestyle interventions for population-level benefit, and cautious, monitored supplement use when clinically justified.
Drivers of the rising interest
Multiple converging forces explain why anti-inflammatory approaches have become a focal point:
- Scientific progress: Better understanding of inflammatory pathways and more sensitive biomarkers make inflammation both measurable and actionable.
- Commercial signals: High-value drug approvals, acquisitions and venture funding in inflammation-related R&D increase visibility.
- Consumer trends: Preventive health, personalized nutrition and wellness marketing push inflammation-related concepts into mainstream consumer language.
- Demography: Aging populations and higher chronic disease prevalence create clinical demand for safe, effective anti-inflammatory interventions.
Voices from research, clinical practice and industry
Researchers emphasize precision: inflammation is not a monolith, and interventions that work in one disease may be ineffective or harmful in another. Clinicians urge careful use of biomarkers, guideline-based prescribing and shared decision-making with patients. Industry highlights market opportunity and continued innovation in drug discovery, but also faces pressure to generate transparent evidence and to address access and affordability concerns for high-cost biologics.
Policy implications: equity, access and evidence
Ensuring that the benefits of anti-inflammatory advances reach broad populations requires concrete policy choices. Three levers matter most: (1) clinical guideline development that incorporates emerging evidence to guide appropriate use, (2) reimbursement strategies and pricing mechanisms that increase access to proven therapies, and (3) public-health investments in nutrition and preventive services to reduce baseline population inflammation through structural change rather than purely clinical interventions.
Without these measures, the economic and clinical benefits of new therapies may accrue mainly to patients and health systems in wealthier settings, deepening health inequities.
Practical guidance for readers
For individuals wondering what to do with this information, practical, evidence-aligned steps include:
- Consult your healthcare provider: Don’t start chronic anti-inflammatory medication or supplement regimens without medical guidance — especially if you have comorbidities or take other medicines.
- Prioritize diet and activity: Adopt dietary patterns associated with lower inflammatory markers (more plants, whole grains, oily fish; less refined sugar and ultra-processed food) and maintain regular physical activity.
- Be critical of supplements: Choose products with third-party verification and clinical evidence; be aware of dosing and potential interactions.
- Ask about testing: If you have chronic disease or risk factors, discuss whether measuring inflammatory biomarkers (like hs-CRP) is clinically appropriate for your care plan.
Frequently asked questions
- What exactly is “chronic inflammation”?
- Chronic inflammation is a prolonged, often low-level activation of the immune system that can contribute over time to tissue damage and disease risk. It differs from acute inflammation (the short-term response to infection or injury) in duration and systemic effects.
- Are anti-inflammatory diets proven to prevent disease?
- Evidence shows consistent associations between certain dietary patterns and lower inflammation markers; randomized trials suggest benefit for intermediate outcomes. However, proving long-term disease prevention requires large, long-duration trials and careful controls, so recommendations focus on healthy, evidence-based dietary patterns rather than definitive prevention claims.
- Can I just take supplements instead of changing my diet?
- Supplements can be helpful in particular situations (for example, omega-3s for specific cardiovascular indications), but they are not a substitute for an overall healthy diet and lifestyle. Quality and dosing vary across products, so professional guidance is recommended.
- Are there risks to targeting inflammation?
- Yes. Long-term NSAID use can increase risks such as gastrointestinal bleeding and kidney damage. Immune-targeting biologics can increase infection risk and require monitoring. Any anti-inflammatory strategy should weigh benefits versus risks on a case-by-case basis.
What to watch next
Expect continued activity across research, clinical practice and consumer markets. Important near-term developments to follow include approvals of targeted inflammation therapies in new indications, publication of large-scale dietary trials that standardize “anti-inflammatory” patterns, and regulatory scrutiny of supplement claims and product quality. How these developments influence prescribing, reimbursement and consumer behavior will determine whether rising interest translates into improved population health or merely a wave of marketing.
Limitations and final notes
This article synthesizes market analysis, published research and public commentary to provide a balanced view of rising interest in anti-inflammatory strategies. Market projections are inherently uncertain and depend on trial outcomes, regulatory decisions and pricing dynamics. Observational research cannot on its own prove causality, and the biological diversity of inflammatory processes means that results in one context should not be overgeneralized to another.
In short: interest in anti-inflammatory approaches is growing for defensible scientific and commercial reasons, but translating that interest into safe, equitable health benefits will require rigorous evidence, thoughtful clinical practice and sensible policy action.